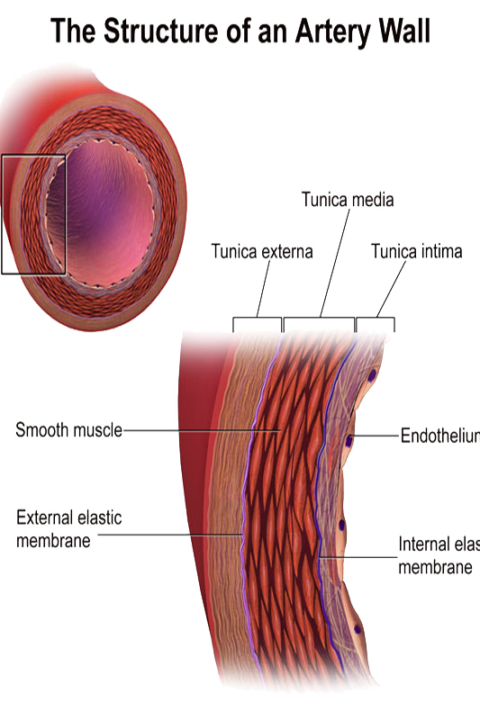
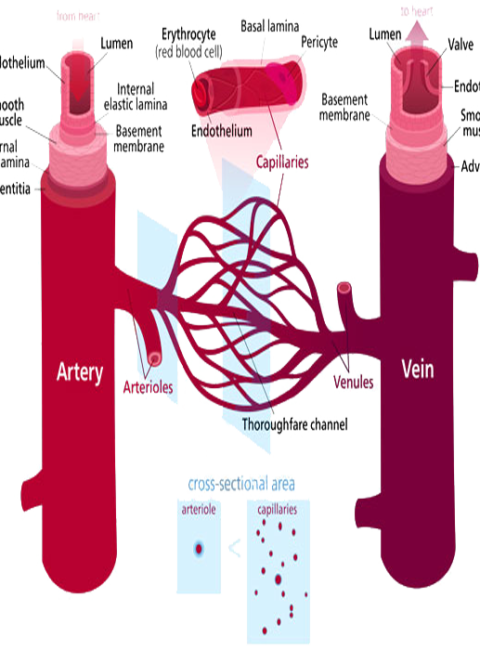
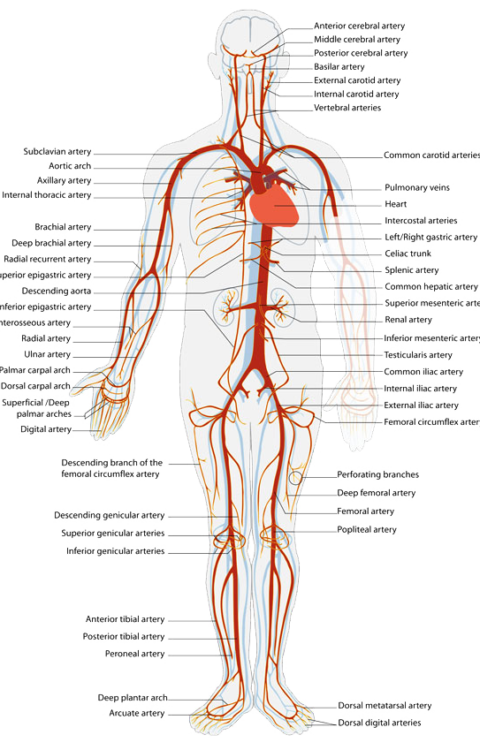
Peripheral vascular disease (PVD), commonly referred to as peripheral arterial disease (PAD) or peripheral artery occlusive disease (PAOD), refers to the obstruction of large arteries not within the coronary, aortic arch vasculature, or brain. PVD can result from atherosclerosis, inflammatory processes leading to stenosis, an embolism, or thrombus formation. It causes either acute or chronic ischemia (lack of blood supply). Often peripheral arterial disease(PAD) is a term used to refer to atherosclerotic blockages found in the lower extremity.
PVD also includes a subset of diseases classified as microvascular diseases resulting from episodal narrowing of the arteries (Raynaud’s phenomenon), or widening thereof (erythromelalgia), i.e. vascular spasms.
Levels of disability are divided into 6 subsets. The classification system, by Rutherford, consists of three grades and six categories:
Mild claudication
Moderate claudication
Severe claudication
Ischemic pain at rest
Minor tissue loss
Major tissue loss
Symptoms
About 20% of patients with mild peripheral arterial disease(PAD) may be asymptomatic; other symptoms include:[1]
Claudication – pain, weakness, numbness, or cramping in muscles due to decreased blood flow,Sores, wounds, or ulcers that heal slowly or not at all.
Noticeable change in color (blueness or paleness) or temperature (coolness) when compared to the other limb
Diminished hair and nail growth on affected limb and digits.